FOR EDUCATIONAL PURPOSES ONLY



https://radiologyassistant.nl/chest/hrct/common-diseases
https://radiopaedia.org/articles/interstitial-lung-disease




https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-018-0643-3
https://www.frontiersin.org/articles/10.3389/fmed.2017.00176/full





https://www.mdcalc.com/isth-criteria-disseminated-intravascular-coagulation-dic
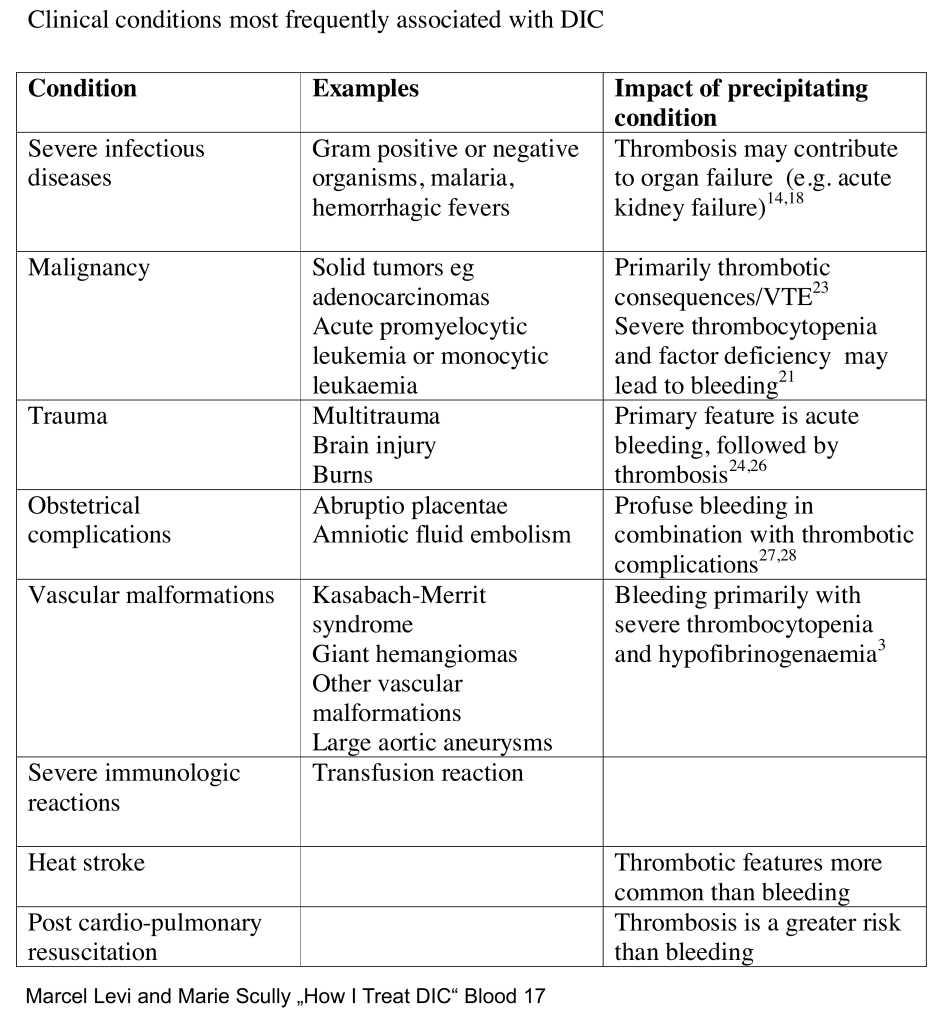






https://onlinelibrary.wiley.com/doi/10.1111/jth.12155
2013
Recommendations:
The threshold for transfusing platelets depends on the clinical state of the patient. In general, platelet transfusions are administered to patients who are actively bleeding and who have a platelet count of <50 × 109 L−1. A much lower threshold of 10–20 × 109 L−1 is adopted in non-bleeding patients, on the basis of RCTs in patients with thrombocytopenia following chemotherapy. Platelets may be administered at higher levels than this in patients perceived to be at high risk of bleeding on the basis of other clinical and laboratory features.
It may be necessary to use large volumes of plasma to correct the coagulation defects shown by prolonged APTT or PT, or a decreased fibrinogen level. Initial doses of 15 mL kg−1 of FFP are suggested, although there is evidence that a dose of 30 mL kg−1 produces more complete correction of coagulation factor levels. In this regard, the consequences of volume overload may have to be considered.
Smaller volumes of PCC may be useful in this setting, although these products lack certain essential coagulation factors, such as factor V. Specific deficiencies in fibrinogen can be corrected by administration of purified fibrinogen concentrates or cryoprecipitate.
The response to component therapy should be monitored both clinically and by repeating platelet counts and coagulation tests following administration of these components.
The efficacy and safety of recombinant FVIIa in DIC with life-threatening bleeding are unknown, and it should be used with caution, or as part of a clinical trial.
_________________________________________________________________________________________________________
_________________________________________________________________________________________________________

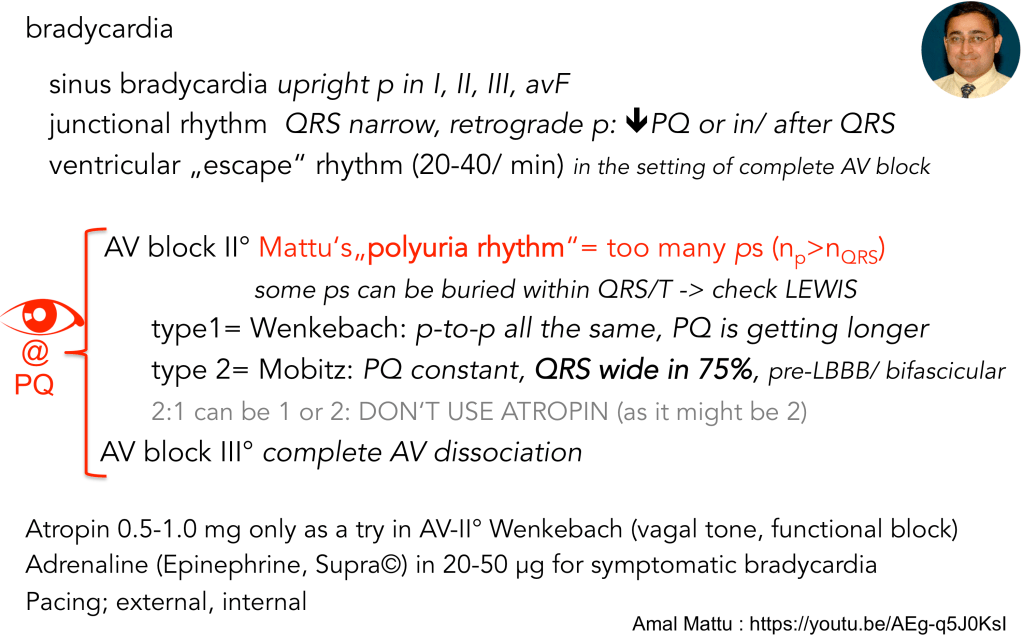
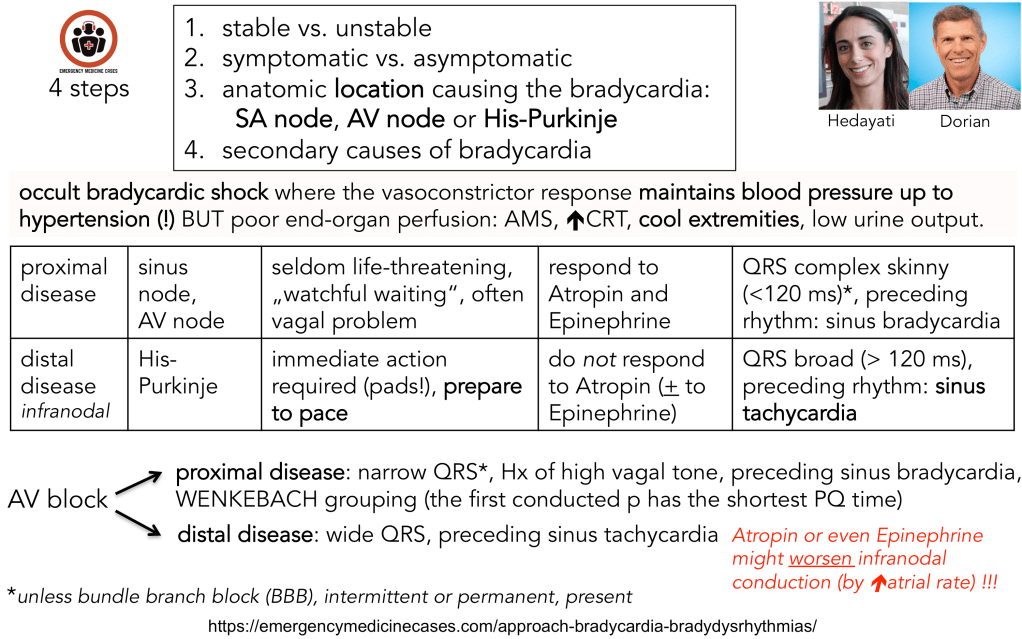
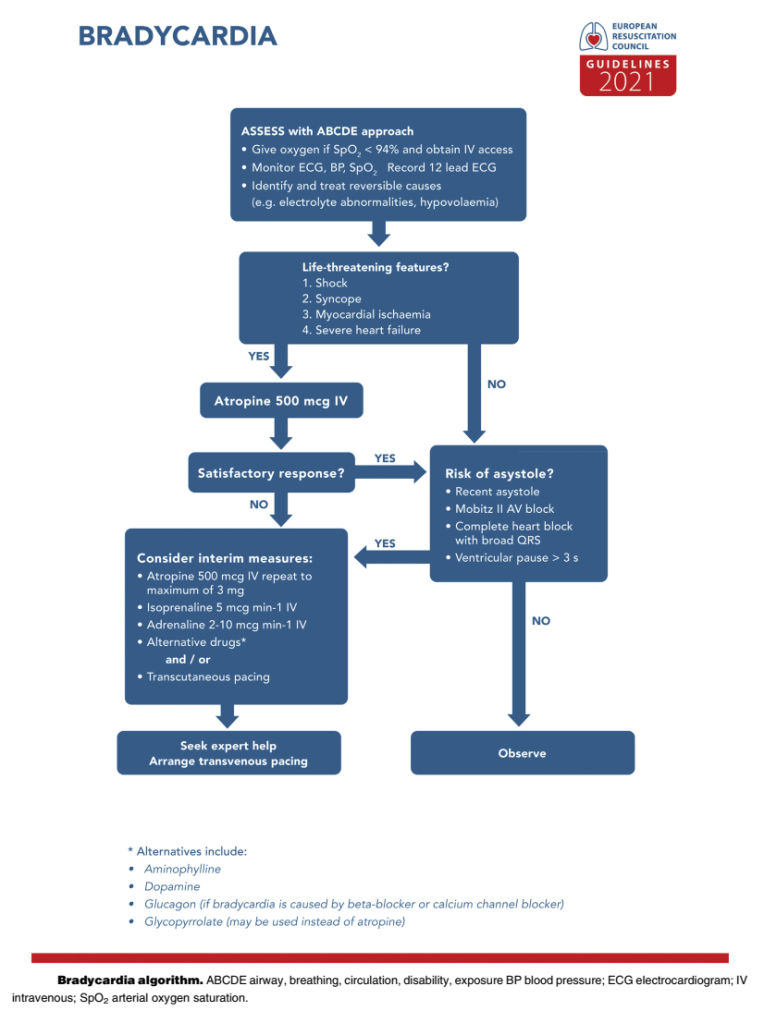
Bradycardia DDx
Seldom, but not miss in any AV blocks:
(1) Lyme
(2) Sarcoid
(3) Chagas
Reply